One of the most notable robotics stories of 2022 was the San Francisco Police Department's decision—and subsequent retraction—to allow roots to use deadly force. By contrast, Tombot addresses another major social challenge—nearly one-third of San Francisco's population is elderly.
This population is the most vulnerable, seeing a 17% increase in Alzheimer’s and dementia deaths with the advent of COVID-19. As the U.S. grapples with an aging population, dementia is becoming one of the largest killers of seniors, greater than breast cancer and prostate cancer combined.
One in three people over the age of 65 die of Alzheimer’s or another form of dementia, according to the Alzheimer's Assocation. The most tragic aspect of the disease is the limited means of treating it.
Many nursing homes have introduced animal therapy sessions for patients. Numerous research studies have found that animals (especially dogs) have improved moods and increased social interaction with residents, especially dementia patients.
Other benefits include decreased anxiety, positive emotions, lower blood pressure, calming effects, and a reduction in aggressive behaviors. However, pets require a lot of care, and with almost 20% of the population allergic to cats and dogs, having a furry friend in a medical facility permanently is impractical.
Paro pioneers robotic therapy
In 1993, Japan’s National Institute of Advanced Industrial Science and Technology started building a robotic companion seal for the country’s rising elderly population, called Paro. Almost a quarter of Japan’s population is over 65, and robots are deployed in a variety of jobs aiding the disabled, including feeding, physical therapy, diet, and exercise coaches. In 2009, Paro received regulatory approval as a Class 2 medical device in the U.S.
The Wall Street Journal reported in 2010 on the use of the animatronic device in nursing homes. As Marlene Dean of Pittsburgh Vincentian homes explained, “Some of our residents need more than we as human beings can provide. We’ve tried soft teddy bears that talk and move. But they don’t have the same effect.”
In fact, Paro has a library of peer-reviewed studies that illustrate the impact of a “robot” that can intuitively track eye movement and recognize users like real pets. For example, at the dementia unit of Vincentian homes, staffers reported significant mood changes when patients started petting the robot.
As Ms. Biro stroked the robot’s synthetic fur, the machine batted its eyelashes and tracked movement with its head and eyes. “I love this baby,” Ms. Biro cooed. Aides also take Paro to residents’ rooms to get them to socialize. At another Vincentian home, Ms. Simmeth, 73, doesn’t always participate in group activities, but she ventures into the hall when she hears Paro’s sounds. “I love animals,” explains Ms. Simmeth. She whispered to the robot in her lap: “I know you’re not real, but somehow, I don’t know, I love you.”
Tombot designed to help people with dementia
Last month, I interviewed Tom Stevens, the inventor of Tombot, the most realistic robotics dog specifically made for the treatment of dementia. He invented the mechatronic canine from the trauma of having to take away his Mom’s dog as she was suffering from dementia.
“I started looking around for substitutes for live animal companions but didn’t find anything that she liked or would respond to,” Stevens recalled. “So I started wondering if technology might play a role that launched me on a multi-year research and education journey which culminated in a master’s degree from Stanford.”
“Along the way, I learned that my mom’s story isn’t unique, that there are tens of millions of seniors around the world with dementia and about a billion people in total that suffer from some form of serious mental health adversity, and due to their condition they aren’t able to successfully care for a live animal,” said Stevens.
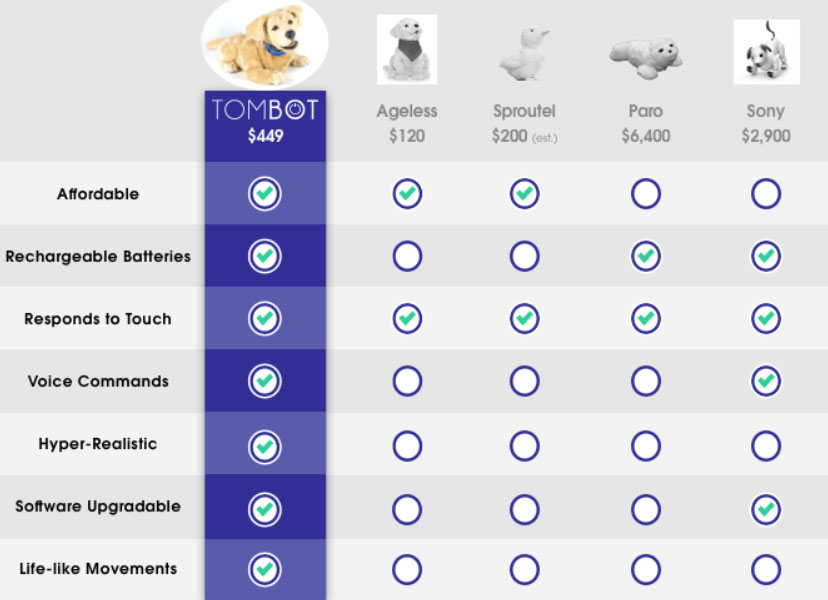
While Paro invented the idea of robotic animal therapy, $6,000 is a lot of money for health institutions and individuals to pay for such a device.
Jennie is next-gen product
Tombot’s latest product, a golden retriever named Jennie, has been shown to reduce stress and violent behavior. Stevens explained that seniors with dementia suffer from emotional detachment as their conditions worsen with loneliness, frustration, anxiety, hallucinations, and in Stevens’ mother’s case, violent anger. To date, the medical establishment has relied on harmful psychotropic and opioid medications to ease the condition.
However, Stevens’ approach is about using the patient’s oxytocin production to treat these mental health illnesses by simulating the emotional support of a dog. Testing out the concept, he said, “we conducted multiple rounds of customer studies with hundreds of seniors with dementia, and what we learned is that they have a very strong preference for realism and things that they’re familiar with. So dogs and cats.”
Based in Los Angeles, Stevens sought out Holywood’s award-winning special effects studios to provide realism to Jennie.
“We teamed up with The Jim Henson Co., the people behind Sesame Street, to do all of our artistic design, and with their support, we are building what we believe to be of the world’s most realistic animals, scientifically designed to stimulate emotional attachment,” shared Tombot's creator. “And then, once that emotional attachment is in place, we become the ideal platform for monitoring that senior for safety and health purposes.”
While Jennie looks like a plush stuffed animal, she’s packed with an enormous amount of technology.
“We did a lot of research and understanding about what it is about dogs that people notice, and what makes them attractive,” explained Stevens. “Unlike [Boston Dynamics'] Spot, Jennie is a lap dog with its feet immobile. One of the first things we learned is that anything on the ground presents an extreme tripping hazard for a senior with dementia, and a fall event for a senior with dementia is frequently an end-of-life injury.”
He suggested thinking about a robot from the lap dog perspective and the opportunities of being so close to the patient with lots of sensors monitoring their every move.
“So, we covered her with sensors and she can feel how and where she’s being touched,” Stevens said. “You can tell the difference between a simple touch, a slow caress, a vigorous pet, and being held. She responds to voice commands. We came up with a smartphone app that allows people to do a number of initial configuration settings to customize the robot, so it will respond only to a given name.”
He then demonstrated Jenny live for me on Zoom utilizing the microphones, sound localization, touch sensors, accelerometers, and gyros. Jennie also comes equipped with a wireless charging blanket, where she rests at night. And when the lights go out, she immediately knows not to bark.
Robot can collect useful data
In addition to treating the patient by increasing their emotional attachment, medical professionals can also use the same platform for monitoring changes in behavior, diet, and living conditions.
“All connectivity is through Bluetooth,” said Stevens. “That’s where the robot gets updates and all the communications. It’s also where it communicates back to the smartphone.”
He elaborated on his product roadmap to use this monitoring information to be able to monitor Sundowning syndrome in dementia patients. This condition is where seniors start to be confused or disorientated at the end of the day, to date it has been poorly understood. Tombot is currently working with the Cleveland Clinic to design a doctors’ user interface to analyze patient data.
Insurance reimbursement a challenge
In addition to the sophisticated sensor platform, Jennie is very affordable for both medical purchasers and consumers. According to Tombot’s Kickstarter campaign (featured in Oprah Daily), the robo-creature will retail for $450. However, Stevens is not satisfied with that amount, as he wants it accessible to everyone. Therefore he is working on acquiring insurance reimbursement.
“We intend to use clinical studies. We’re going to market it as a wellness device, a non-regulated device. We intend, however, starting with the beta to conduct clinical studies with our research partners at Children’s Hospital of LA and the Children’s Hospital of Orange County to measure changes in oxytocin levels.”
These efficacy trials could open up treating other psychological disorders, including depression, anxiety, bipolar, schizophrenia, chronic pain, and autism. Oxytocin is difficult to measure, as it doesn’t pass readily through the brain’s blood barrier and saliva is not very accurate.
“These children’s hospitals have very large patient populations with neurosurgical patients,” said Stevens. “And these kids have shunts in their heads that bleed off the excess cerebral spinal fluid to prevent swelling of the brain’s inner-cranial area. So we can non-invasively tap into that spinal fluid and monitor changes, and the oxytocin levels that correlate to interactions with the robot.”
Stevens then claimed that his device will be “the first of any kind approved by the FDA for oxytocin. And with that, we will get Medicare and Medicaid reimbursements.”

About the author
Oliver Mitchell is a partner at ff Venture Capital. His areas of focus are drones, robotics, and applied AI. Mitchell is also an adjunct professor at Yeshiva University. This column is reposted with permission.
Mitchell is traveling this week to CES; anyone interested in meeting can reach him on LinkedIn.
Article topics
Email Sign Up
















